
The cloud-based system offers robust financial reporting, automated claim submissions, and customizable billing workflows to maximize revenue efficiency. The EHR integration ensures smooth data synchronization between clinical and financial operations. The system provides advanced billing automation with a Accounting For Architects 98% first-pass acceptance rate, enabling providers to accelerate reimbursements. In-house billing solutions give practices complete control over revenue cycle operations, while outsourced billing services offer professional support for claim submissions and follow-ups. Patient engagement tools such as telehealth, online scheduling, and digital payments enhance accessibility and improve the overall patient experience. Identifying the root cause of the denials helps healthcare providers to initiate the right steps to resolve them.

What if I have concerns about losing control over my billing processes?
![]()
First-pass acceptance is also called a “clean claim,” and it is one of the best ways to measure the efficiency of your billing cycle. The other codes used in medical billing are Current Procedural Terminology (CPT) codes, developed by the American Medical Association (AMA). These CPT codes refer to the treatments administered by the practitioner, making them vital to ensuring accurate reimbursement for services rendered. Below, read summaries of five of the leading platforms followed by a link to a full review of each. In this case, your billing team should review the payer’s decision, which will often be detailed, for potential inaccuracies. If you spot any errors, you can begin the appeals process, although it can be costly and lengthy.
Software for Medical Billing to Simplify Your Revenue Cycle
- The payment posting step influences many other functions of the medical office and can altogether influence patient satisfaction, efficiency, and overall financial performance.
- If there are errors, the claim will be denied, although a detailed explanation and steps to rectify any issues will be included.
- Each step builds upon the previous one, creating a seamless flow from initial patient contact to final payment collection.
- Inquire about deductibles, copays, coverage and benefits so that you know how much to collect from the patient.
- This involves generating an invoice or statement that details the balance due, due dates, and payment methods.
- With these instructions, you can refile your claims quickly and (hopefully) be reimbursed.
- Once the payer has paid their share, the remainder owed is passed onto the patient in a separate statement.
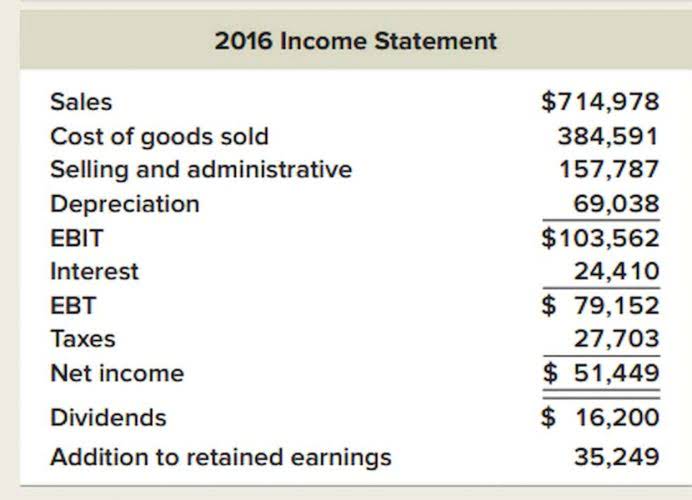
Our platform makes income statement it easy to create a win-win situation for patients and providers. By ensuring transparent and timely communication of financial information, practices can build patient trust and streamline revenue collection processes. The exception to this rule is high-volume payers, like Medicaid, who will acknowledge claims directly from healthcare providers.

Job Outlook for Medical Billing and Coding Specialists
CharmHealth’s scalable design accommodates both small clinics and large physician groups, ensuring flexible and cost-effective implementation. By outsourcing, healthcare staff can focus on patient care rather than paperwork, leading to improved service quality. Together, medical billing cycle steps they may ensure that all healthcare professionals and providers are accurately paid for the services they provide. Proper modifier use, such as -LT, -RT, and -59, differentiates procedures, preventing bundling errors and ensuring maximum reimbursement for complex orthopedic treatments.

Now the insurance company processes the claim, again reviewing information and making sure that all billed services are ones they are bound to cover according to their contract with you. Denial can result from simple errors, but in this case, they will also explain their judgment and the steps you’ll need to take to set things right. Still, this is costly in terms of putting your staff back to work on a claim that appeared finished, as well as the delay in payment. Any mistakes made here can be costly, resulting in a denied or delayed claim, so be sure your medical script is free of errors, and your coding team is tip-top and up-to-date on the current codes.
- Automation, billing software, and electronic health records (EHR) are essential in contemporary medical billing.
- Many insurance providers and medical providers have agreements with how much each procedure will cost.
- Identifying vulnerabilities early helps maintain a high standard of reliability and security in the final product.
- This crucial aspect of medical billing and revenue cycle management plays a significant role in ensuring financial sustainability for healthcare providers.
- A structured approach ensures efficiency and accuracy from defining requirements to development and post-launch maintenance.
Best medical billing software
Otherwise, you’ll need to alert the patient to their financial responsibility, ideally before their appointment. Choose a partner that is HIPAA compliant or follows equivalent data protection regulations. They should have robust security measures, such as data encryption, secure servers, and access controls. Connext Global Solutions ensures HIPAA compliance through biometric access, 24/7 IT support, and virtual desktop environments where no client data is stored locally.